

Med+ safe
What is Med Safe?
Med Safe was designed to aid medication compliance by reducing the medicine-related information load on the multiple medication consumers. For patients who are prescribed multiple medications, considerable deliberations and calculations about dosage, frequency and drug types were made beforehand to prevent critical drug interactions; therefore, taking just any mix of medications (over-the-counter or prescribed) in these cases may cause unwanted symptoms or interference with other treatments. However, the information load can be burdensome for elderly multiple medication users, especially because the information is often provided in forms of dense brochures packets, one-time training before discharge or via personal web searches.
Med Safe is a multi-functional engineered pillbox that addresses medication noncompliance in two ways:
1. keep medical record and medication regimen
2. ensure the compatibility of additional medications such as over-the-counter (OTC) medications
Why Med Safe?
Many studies show that medication noncompliance is a common problem for pharmacists and doctors. In the US, about 3.8 billion prescriptions are written each year, but over 50% of them are taken incorrectly or not at all [1]. Of these 3.8 billion prescriptions, 20% to 30% are never filled. For elderly patients, noncompliance is estimated between 40% and 75% [3]. Furthermore, medication compliance plummets after six months. Depending on the medication, this drop can be as high as 66% [1, 2].
Common reasons for noncompliance include patient forgetfulness, altering his/her own schedule or dosage, and cost concerns. Elderly patients are more likely to be forgetful when they are taking multiple medications simultaneously, and a study of 10,000 patients found 24% of noncompliance was due to forgetfulness [1, 3]. This same study found that 14% did not feel a need to take their medications due to a belief that the medications would have little or no effect on their condition.
Problem scenario
An elderly man, who turned 72 this year, is currently taking medication for blood pressure, osteoporosis, and arthritis. Since last night, his head has been throbbing, can he take aspirin?
Team: Power Group




CS student, PhD
ISE student, MS
ISE student, MS
CS student, MS
Phase of the Project
Research
Analyze
Conceptualize
Prototype
User Test
Iterate
A new design project from scratch!
My role...
Research
In order to remain in accordance with the Health Insurance Portability and Accountability Act (HIPAA) and the Institutional Review Board (IRB), contextual data gathered through semi-structured interviews from caregivers and pharmacists were not recorded in any fashion outside of note-taking. Furthermore, no observations were made during the contextual inquiry. Due to these limitations, information regarding multiple medication users (MMUs) came solely from the aforementioned secondary sources, and questions were kept general when discussing MMUs.
For an abridged contextual inquiry, we used snowball technique to recruit one in-patient and one out-patient pharmacist, whom we defined as our subject matter experts (SMEs). The probing questions in our semi-structured interviews provided a comprehensive understanding of the work practice. Three interviewers were present during the interviews, two took extensive notes and the other moderated the questions.

Analysis
After completion of the contextual inquiry, we transferred the notes to sticky notes and constructed a work activity affinity diagram (WAAD) to better organize the interview notes, to understand how the current domain in medication scheduling works, and to visualize the magnitude of certain concerns and potential cross-sectional problems to aid our future design implications and design feature prioritization. After categorization of the findings, we created a flow model, which included aspects of a social model to inform future design decisions based on the identified user needs to illustrate the exchange of drug information between the identified work roles, the type of information being transferred, and the interaction between the system and its users. The flow model was also effective in highlighting the barriers in the current system. The results of the analysis informed future personas and design decisions based on the identified user needs.





Conceptualize
After completing the contextual analysis, we used the information identified by the completed WAAD and flow model to construct a set of personas and perform rapid sketching based on the 3 main design implications.
Barrier 1.
Lack of communication among multiple doctors who prescribe different medications for specific conditions
Design implication 1.
Use of a central portable memory card that is compatible with the hospital medical record software, enabling easy updates by doctors during visits
Barrier 2.
Lack of appropriate inquiries from the multiple medication users about the drugs they are consuming
Design implication 2.
A shared database of medicine reaction with the pharmacists for viewing only, accessible by the Med Safe app
Barrier 3.
Poor method of drug information communication (e.g. thick documents and wordy pamphlets)
Design implication 3.
A feature that compares the searched (or barcode scanned) to the saved record of the patient's drug regimen.
For the personas, we utilized the concept of a primary user class in discussions concerning our final design in Persona Priority Matrix. We based this decision on information gathered from inpatient and outpatient pharmacists, who stated that the systems they are currently utilizing work well for their purposes, and both pharmacists recognized that the true need lies in improving medication compliance for elder independent MMUs. .
Personas
For the personas, we utilized the concept of a primary user class in discussions concerning our final design in Persona Priority Matrix. We based this decision on information gathered from inpatient and outpatient pharmacists, who stated that the systems they are currently utilizing work well for their purposes, and both pharmacists recognized that the true need lies in improving medication compliance for elder independent MMUs. .



Sketching (Low-Fidelity)
We agreed that a stationary interface such as a desktop computer would not be helpful for our primary persona of independent MMU, who are more likely to experience mobility problems. However, we also realized that many MMUs will not have access to a smart mobile device (e.g. smartphone). As a result, we designed a standalone interface (main system) for medication management with a wearable that syncs to the system. The interface design will be tailored towards simplicity with large icons and words to facilitate ease of use and increase visibility of information.



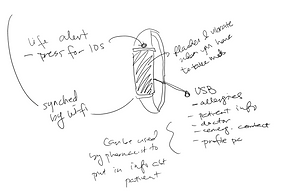
Moreover, because our interview results showed that many of our MMUs utilize and prefer traditional pillboxes, we chose not only to use this as a metaphor to conform to the MMU’s mental models but also to incorporate the pillbox as part of the functionality, designing an enhanced pillbox, which will be be mechanized and digitalized for ease of use. The pillbox will take digital input from the pharmacy system about medication dosage and frequencies and will automatically sort the MMU’s medications based on this information. The normal state of the box is closed which allows for automatic dispensing. Should the MMU wish to access the dispensed medication manually (e.g. if they need to go somewhere and must take the medication with them), they can open the box and it appears as a normal pillbox with the same familiar interactions.


Storyboard (Ecological Perspective
Using these sketches, we chose a representative scenario for storyboarding that explored key user interactions and interface features.

Prototype
We developed a high-fidelity prototype with HTML embed in powerpoint, without the back-end infrastructure and database, for the touch interface on the front surface of the enhanced pillbox, similar to a tablet touchscreen. This interface allows the user to interact with the pillbox. In its default state (the MMU is not interacting with it and there are no medications to be administered), the screen will simply serve as a large backlit digital clock. Below are some samples of the interface slides used for evaluation in the next phase.






For the main system, the enhanced pillbox, we created a low-fidelity prototype with a store-bought pillbox and cardboard to imitate the shape of the container. We also used the fit bit as the wearable.

User Test
We assumed that the MMU’s information was already uploaded to both the wearable and the pillbox by a doctor or pharmacist, and focused on the user's interactions with the pillbox interface and the wearable.
We chose to do a rapid analytical evaluation of the prototype via design walkthrough and feedback provided by the domain expert, the outpatient pharmacist, whom we interviewed during contextual inquiry. We chose this method due to lack of accessibility to the target users, the elder MMUs. We also provided 8 benchmark tasks in order to guide the domain expert, who is not necessarily familiar with design evaluations. We collected three types of data: objective-qualitative (critical incident identification), subjective-qualitative (domain expert opinions, open-ended follow-up questionnaire, and subjective-quantitative using a modified USE questionnaire with a five-point Likert scale).
After a brief introduction to our prototype, we asked the pharmacist to perform eight different user tasks with the pillbox. One of these tasks included interactions with the wearable in which we used Wizard of Oz techniques to make the Fitbit vibrate at the desired moment. For each task performed, we took note of any critical incidents encountered. After most tasks, we asked brief follow up questions to gather what he thought about individual features and noted his responses and our observations. Next, we asked the pharmacist to rate our design using a five-point Likert scale. After this rating, we asked him a series of follow-up questions.

Iterate
The critical incidents from the sessions, interviewer's notes and respective design implications based on the recorded data were drawn on a table for future design iterations.


Despite some faults in our initial design, the pharmacist seemed overall pleased with the interface, as demonstrated by his high rankings to our questions and positive responses to our open-ended questions. Furthermore, he felt that the concept would be great if the database was complete and if the pillbox took into account all possible scenarios, such as different pill sizes and various patient conditions.
Challenge
Because of our decision to focus on independent MMUs for our design, we also focused on this user group for our prototype and evaluation. However, this severely limited our pool of possible evaluators. This fact combined with time constraints led us to conduct a single evaluation with one of the pharmacists we had interviewed acting as a domain expert. Additionally, the evaluator was distracted during the evaluation itself, which could be attributed to the fact that the evaluation was conducted during his working hours at his workplace.
While we were able to complete the tasks and the ratings on our design, he completed them as quickly as possible and was unable to finish the open-ended follow-up questions. Instead, we emailed him the follow-up questions to answer at his convenience. As a result, our evaluation of the interface is solely reliant on this pharmacist, which is likely skewed due to his distractions and feelings of being rushed. Therefore, we prefer to engage more evaluators before progressing to the next iteration of development.
"User test at least 5 participants, to find about 80% of the usability fault"
-
N. Chesanow. 2014. The Noncompliance Epidemic: Why Are So Many Patients Noncompliant? Medscape.com. (16 January 2014). Retrieved April 25 from http://www.esculape.com/2014/Why-Are-So-Many-Patients-Noncompliant.pdf
-
Farah M. Chowdhury, Deesha Patel, Mary G. George, David Callahan. 2013. Medication Adherence. CDC Conference. (27 March, 2013). Retrieved April 27, 2016 from http://www.cdc.gov/primarycare/materials/medication/docs/medication-adherence-01ccd.pdf
-
C. Salzman. 1995. Medication compliance in the elderly. In J Clin Psychiatry. Retrieved April 25 from http://www.ncbi.nlm.nih.gov/pubmed/7836347